What Causes Light Bladder Leakage?
Why am I Experiencing Bladder Leaks?
Women’s bodies are full of surprises – leaking urine is no exception. In fact, you might be surprised to know that 1 in 3 women experience bladder leaks. The risk factors and causes of bladder leakage, also known as urinary incontinence, vary from person to person. Although urinary incontinence can cause feelings of loneliness or embarrassment, it is often very treatable.
Are there different types of bladder leakage?
The most common type of incontinence in women is stress incontinence, which occurs when urine leaks out due to sudden pressure on the bladder and urethra, causing the sphincter muscles to open briefly. Pressure from sudden forceful activities like exercise, sneezing, laughing or coughing can trigger stress incontinence to occur.
Another type of incontinence in women is urge incontinence, or detrusor instability, which occurs when the nerves feeding the bladder wall muscles fire when they shouldn’t, giving one the sudden urge to go. This is combined with the nerves feeding the pelvic floor muscles telling them to relax, and the result is bladder leakage.
It is not uncommon for someone to experience a combination of both, referred to as mixed incontinence. Some women have an over-distended bladder that, much like a stretched-out balloon, is unable to contract well and stays too full, resulting in overflow incontinence. Others may have weakness in the muscles of the urethra that are necessary for keeping urine in the bladder, or intrinsic sphincter deficiency.
Causes of bladder incontinence
There are many women who may experience some mild and occasional leakage and find themselves asking “why am I leaking urine”?
So, what causes bladder leakage? Often, weakened pelvic floor muscles due to general health or lifestyle changes can cause bladder leaks. Other times, muscles may be strong, but lack proper coordination. Pelvic health physical therapists can help patients maintain a well-functioning pelvic floor to control urinary functions.
There are various life events that can cause incontinence including:
•A Previous Pregnancy or Childbirth. Many of my patients don’t realize that pregnancy can increase their risk of pelvic floor dysfunction due to the pressure being put on the pelvic floor, regardless of how you deliver. The pelvic floor, which are muscles that control bladder and bowel movements, are stretched over 300% during vaginal delivery. This is one factor which increases your risk of pelvic floor dysfunction. However, since pregnancy itself causes postural (relating to your posture) and hormonal changes, these can also increase the risk of bladder leaks. That’s why I recommend all women to have a plan for postpartum pelvic floor physical therapy.
•Getting Older with Less Bladder Control. As women enter menopause, estrogen production starts declining. Estrogen keeps the cells of the bladder, urethra and vaginal lining healthy, but during menopause, many women experience Genitourinary Syndrome of Menopause (GSM). This is a new term that encompasses both atrophy and urinary symptoms associated with menopause and a lack of estrogen. This may cause sudden or worsening incontinence. This also contributes to the loss of support in the bladder and weakness around the urethra. Frequent bathroom trips increase as women get older due to bladder capacity reducing with age. Along with menopause, there are many other bladder leakage causes from various medical disorders such as hypertension, vascular disease, neurological disorders and diabetes.
•Hysterectomy. A total hysterectomy, which is a surgical procedure to remove the uterus, will result in the same physiologic changes and resulting symptoms as above. However, if it is done prior to menopause, these changes will be much more sudden.
Certain medications can also contribute to incontinence, including many cardiovascular medicines and diuretics, sedatives, muscle relaxants and Parkinson's treatments. Medical and neurological disorders that can also result in bladder leakage include:
- Diabetes
- Multiple Sclerosis
- Parkinson's Disease
- Spinal injuries
- Connective Tissue Disorders
- Urinary Tract Infection
- Interstitial Cystitis
- Kidney Stones
- Bladder Cancer.
What treatment options exist for incontinence?
Bladder leakage treatment options will be different based on your individual needs and knowing how to manage leaks.
1. Track your triggers
Woman experiencing bladder leaks all have their own triggers that can bring on leaks. To best determine what may be triggering you, track your food, drinks, and activities and look for any developing patterns that may arise. Some dietary irritants include:
- Alcohol Consumption
- Caffeine Intake
- Carbonation
- Sugary foods, such as honey
- Artificial Sweeteners
- Acidic Foods such as citrus
- Spicy Foods
- Tomato-based foods (yes, that red sauce on your pasta counts!)
- Chocolate
2. Monitor your fluid intake
Keep your bladder healthy and try to drink six to eight 8-oz glasses of water a day. When you drink less water, your urine becomes more concentrated and may irritate the lining of the urethra and bladder. This can cause bladder spasms and unexpected leaks.
3. Talk to your doctor and pelvic health physical therapist
Getting advice specific to your symptoms offers the best chance of reducing or even eliminating bladder leaks. To make the conversation easier, write down and share the following things: what time and with what activities you leak, how often you leak, how much you leak, and any triggers that cause you to leak. This will help your doctor determine the best treatments.
4. Strengthen your muscles
Strengthening the muscles of your pelvic floor and surrounding muscles can help reduce leaks with the support of a pelvic health physical therapist. Pelvic health physical therapy is a non-surgical option that's highly effective and supported by tons of research. Since bladder leakages and your pelvic floor go hand in hand, pelvic health physical therapists are great go-to specialists to seek. They may suggest pelvic floor exercises, such as Kegels, to practice strengthening your pelvic floor, but will also evaluate you for other contributions to your bladder leakage.
5. Manage leaks
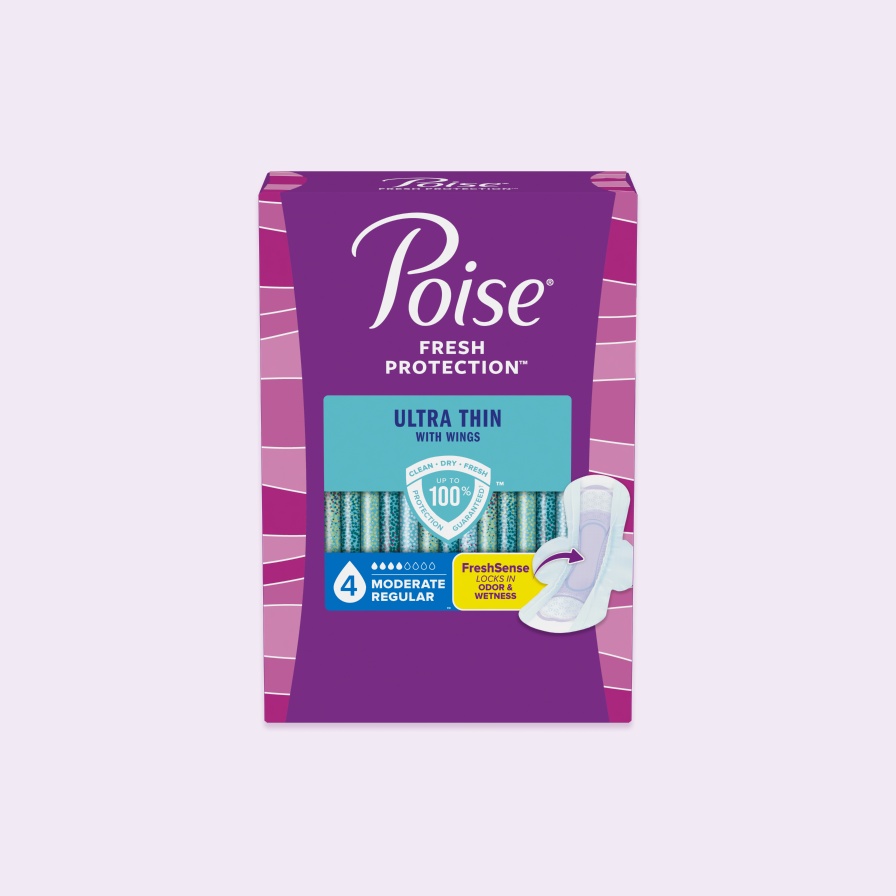
Poise® offers expert protection for bladder leaks to help keep you dry and comfortable. Each product is slightly different to help solve your specific needs and help put you back in control of those sneaky bladder leaks. Products best suited for urinary incontinence include:
- Poise® Ultra Thin Pads – The brand’s thinnest pads wick away moisture and odor for all day protection. Available with stay-in-place-wings or without, they keep you 10x drier than the leading period pad so women can be their true selves without worrying about bladder leaks.
- Poise® Impressa® Bladder Supports – These are inserted and removed the same way as a tampon. Designed to comfortably and discreetly help stop leaks before they happen, and let you enjoy life without a pad.
- Poise® Original Pads – These pads are specifically designed for light bladder leakage and to keep you clean, dry and fresh all day. The ContourFIT® design fits your curves, so you get coverage where you need it, without any bunching or bulking in the middle.
- Poise® Daily Liners – These incredibly thin liners have an asborb-loc® core that quickly locks away wetness and odor while the CleanFresh™ Layer instantly dries to keep you fresh and dry all day.
Author Summary: Dr. Heather Jeffcoat,DPT, Pelvic Health Physical Therapist is the founder of Fusion Wellness & Femina Physical Therapy(FeminaPT.com).Her work focuses on pelvic and sexual health education for all, and she lectures internationally on Female Sexual Dysfunction and chronic pelvic pain. She is also the author of Sex Without Pain: A Self Treatment Guide to the Sex Life You Deserve.
Recommended Products
Absorbency Level
Absorbency Level